The views expressed in this presentation do not represent the official policy or opinion of the United States Navy, Defense Health Agency, Department of Defense, or the United States Government.
Surgical education is on the precipice of a revolution. Over the last several decades, multiple factors such as work hour restrictions, increasing case complexity, decreasing case volume, quality improvement initiatives and rising non-clinical responsibilities have slowly reduced the amount of time surgical trainees spend in the operating room.1,2 In response, a paradigm shift has occurred whereby traditional time-based programs are being replaced with competency-based training systems. Despite this response to the changing surgical education landscape, there remain concerns that today’s training systems produce surgeons who are ill-prepared upon completion of their training.3
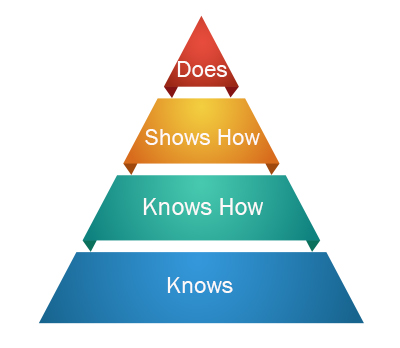
At the crux of the issue lies the fact that successful surgical training requires the development of specialized psychomotor skills, coupled with a mastery of three-dimensional anatomy; a feat that requires training programs to both adapt deliberate practice techniques and provide the tools necessary for mastery. While deliberate practice is often simplified to the public belief that mastery requires “10,000 hours” of practice, this limited view of deliberate practice recognizes that a time-based component is required to develop high-level psychomotor skills.4 In fact, both time spent in deliberate practice and formal rehearsal are key components of Miller’s pyramid, an approach that represents a foundational theory for modern medical education (Figure 1).5 In this approach, the trainee moves from “Knows” to “Knows How” to “Shows How,” before finally arriving at “Does.”5 While on first glance this may seem similar to the tongue-in-cheek saying of “See One, Do One, Teach One,” this theory represents a deliberate process wherein a trainee must first develop the appropriate anatomic and physiologic knowledge, then demonstrate the appropriate application of this knowledge, before finally being allowed to independently apply this knowledge or psychomotor skill to a patient.
But where does this practice fit in the future of surgical education? Since the time of Vesalius over 400 years ago, we have been training and practicing on cadaveric specimens. Unfortunately, repetition and cost make cadaveric specimens an impractical solution for supplementing surgical training as time spent in deliberate practice decreases. Furthermore, as surgical interventions become more complex and nuanced, cadaveric recreations struggle to offer accurate representations of the handling of living tissue. In order to make cadaveric training more realistic, Grabo et al have implemented a perfused cadaver model into general surgery trauma training.6 They showed a retained sense of confidence in their residents who trained on this model when learning and practicing trauma procedures. While a perfused model offers a more realistic training environment, it still requires a cadaver with its incumbent cost that enables a single use. Other groups and companies have developed non-cadaveric based training tools. These tools often focus on developing certain psychomotor skills and offer the ability for repeated use at a fraction of the cost of cadaveric work. In many settings, however, the abstract skills that are developed with these tools may not directly translate to individual patient anatomy and pathology.
Virtual reality (VR) offers a pathway to the future of surgical education.7 VR can provide a safe, low-stakes environment for a trainee to study three-dimensional anatomic relationships and develop the appropriate psychomotor skill sets before entering the operating room.8-9 Additionally, given the digital nature of these systems, they can be tailored to individual patient pathologies, allow for the completion of entire surgeries rather than isolated tasks and be reused at low costs (after initial acquisition costs) to allow for an increased number of rehearsals by one or several trainees. This increased practice can lead to surgical expertise and mastery, resulting in improved patient outcomes.10 We must not forget that a mere increase in the hours of practice is insufficient for competency development. Deliberate practice requires repetition, which is enhanced through feedback and subsequent refining of performance.11 Notably, current technologies in VR can provide this dimension as high-fidelity VR incorporates haptic feedback in addition to visual and aural cues and objective feedback measures that can be incorporated into the simulation.12-13 Imagine a world in which a neurosurgical resident reviews a patient’s case and practices the procedure while receiving feedback that allows for refinement of skills on a model that is patient specific and matches the patient’s anatomical and pathological condition. That technology is now available and has the potential to revolutionize surgical training and improve patient outcomes. It is our challenge now to embrace and incorporate these technological advances into training programs, providing the building blocks for deliberate practice in neurosurgical education.
References
- Fairfax LM, Christmas AB, Green JM, Miles WS, Sing RF. Operative experience in the era of duty hour restrictions: is broad-based general surgery training coming to an end? Am Surg 2010;76(6):578-82. (https://www.ncbi.nlm.nih.gov/pubmed/20583511).
- Malangoni MA, Biester TW, Jones AT, Klingensmith ME, Lewis FR, Jr. Operative experience of surgery residents: trends and challenges. J Surg Educ 2013;70(6):783-8. DOI: 10.1016/j.jsurg.2013.09.015.
- Mattar SG, Alseidi AA, Jones DB, et al. General surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship program directors. Ann Surg 2013;258(3):440-9. DOI: 10.1097/SLA.0b013e3182a191ca.
- Ericsson KA, Krampe RT, Tesch-Römer C. The role of deliberate practice in the acquisition of expert performance. Psychological review 1993;100(3):363.
- Miller GE. The assessment of clinical skills/competence/performance. Acad Med 1990;65(9 Suppl):S63-7. DOI: 10.1097/00001888-199009000-00045.
- Grabo D, Bardes J, Sharon M, Borgstrom D. Initial report on the impact of a perfused fresh cadaver training program in general surgery resident trauma education. Am J Surg 2020;220(1):109-113. DOI: 10.1016/j.amjsurg.2019.10.033.
- Fiani B, De Stefano F, Kondilis A, Covarrubias C, Reier L, Sarhadi K. Virtual Reality in Neurosurgery: “Can You See It?”-A Review of the Current Applications and Future Potential. World Neurosurg 2020;141:291-298. (In eng). DOI: 10.1016/j.wneu.2020.06.066.
- Bernardo A. Establishment of Next-Generation Neurosurgery Research and Training Laboratory with Integrated Human Performance Monitoring. World Neurosurg 2017;106:991-1000. (In eng). DOI: 10.1016/j.wneu.2017.06.160.
- Harrop J, Lobel DA, Bendok B, Sharan A, Rezai AR. Developing a neurosurgical simulation-based educational curriculum: an overview. Neurosurgery 2013;73 Suppl 1:25-9. DOI: 10.1227/NEU.0000000000000101.
- McGaghie WC, Draycott TJ, Dunn WF, Lopez CM, Stefanidis D. Evaluating the impact of simulation on translational patient outcomes. Simul Healthc 2011;6 Suppl:S42-7. DOI: 10.1097/SIH.0b013e318222fde9.
- Ericsson KA, Prietula, M. J., & Cokely, E. T. The making of an expert. Harvard Business Review 2007;85:7/8:114.
- Arikatla VS TM, Enquobahrie A, Nguyen T, Blakey GH, White R, Paniagua B. . High fidelity virtual reality orthognathic surgery simulator. InMedical Imaging 2018: Image-Guided Procedures, Robotic Interventions, and Modeling. International Society for Optics and Photonics 2018;10576.
- Hoogenes J ME. Simulation Surgical Models: Surgeon Perspectives.: Chandos Publishing., 2016.








