
The generally accepted ratio for a sufficient neurosurgical workforce arises from a 1975 government proposal of one neurosurgeon per 100,000 U.S. population (7). More recent analyses place the current ratio at around 1:61,000, and with a growing and aging population, it actually appears this improved proportion may still be inadequate to meet current health care needs (2,4). A 2012 statement from organized neurosurgery thoroughly detailed this problem and suggested actions to be taken to correct it (5).
One of the greatest limitations facing the inadequacy of the neurosurgical workforce is the inability to produce a sufficient number of trained neurosurgeons in a suitable amount of time. With up to 18 years between the start of medical school to the time of board certification, there is too great a delay in providing reinforcements to our workforce. Although there is now a greater emphasis towards subspecialization in neurosurgery, these additional years spent in fellowship training may further complicate the future shortage. Perhaps, a more radical approach should be taken to our training paradigm to provide for better neurosurgical coverage.
Workforce Shortage
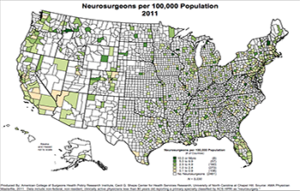
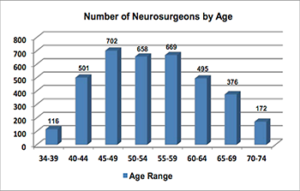
There are over 5,700 hospitals in the U.S. with less than 3,700 neurosurgeons. As neurosurgical services tend to be clustered in areas of greater population density at hospitals with facilities able to accommodate the highly technical aspects of the surgical discipline, many areas of the country are without neurosurgical coverage. This has obvious implications on emergency and trauma care in these regions (3). Additionally, while the U.S. population continues to grow, especially its elderly component, the group of working neurosurgeons is also aging, with almost half of those practicing being 55 years old or greater.
To fill the gap created by a neurosurgical workforce, 102 accredited neurosurgical residency training programs in the U.S. with approximately 1,200 total trainees produce 160 graduates annually. At this current rate, the supply-demand mismatch will grow with time. Simply creating more residency positions will not close the gap quickly enough due to the prolonged length of time required to generate board-certified neurosurgeons. This is further complicated by neurosurgery’s shift towards subspecialization, further delaying new arrivals to the workforce by an additional one to two years.
Creation of a ‘General’ Neurosurgeon
Subspecialization in neurosurgery has arisen out of the significant advances in scientific knowledge and surgical techniques, making it nearly impossible for individual surgeons to stay abreast of all changes in the discipline. “Centers of Excellence” have resulted in regionalization, where subspecialized surgeons and hospitals can maintain higher volumes and, often as a result, better outcomes (6). It has even been proposed to change residency curriculums to better reflect this evolution in neurosurgical training towards subspecialization. One such suggestion involves limiting the number of years (four) spent learning “core neurosurgery,” and then dedicating the mandatory remaining time (up to three years) to subspecialty training (7).
Perhaps, an additional alternative pathway should be considered in hopes of better bolstering the active neurosurgical workforce. To streamline training, a limited number of spots could be created in which residency is restricted to as few as four years in which the core principles of neurosurgery are learned. This would include neurotrauma and the most common neurosurgical procedures. These residency positions could be offered with a stipulation that, upon completion of the shortened training, the graduate would accept a position in an underserved area for a defined period of time. This would provide better access to care and might have the greatest role in trauma or cases of acute pathology, where stabilizing treatments could be performed by these surgeons in a timely fashion before patients are then referred to tertiary care centers.
Such a pathway for creation of “general neurosurgeons” could only be effective if the graduates were to be closely monitored in terms of limiting the procedures that could be performed and requiring that more complex pathologies be referred to larger centers. Continued education beyond graduation would be necessary to maintain abreast of innovations in diagnostics and therapeutics. Simulation, online education and courses similar to the current Neurological Surgeons Boot Camp could be utilized for this purpose. If additional future training were to be obtained, then further privileges could be granted appropriately.
Obstacles
Realistically, any scenario that requires the shortening of residency training is unlikely to be strongly considered at a time when vehement arguments are being made for just the opposite. The institution of work-hour restrictions and the increasing complexity of the health care system and neurosurgical procedures has prompted many to worry that seven years may not in fact be long enough to create a meaningful foundation of knowledge and technical proficiency. Despite this, a radical approach will likely be necessary to address the future neurosurgical workforce shortage. Further prolonging residency, as suggested, particularly when pursuing additional years of advanced fellowship training has become so prevalent, will likely only thrust us further into an impending neurosurgical health care crisis.
References
1. Barrow, D.L. (2013). Subspecialization in Neurosurgery. World neurosurgery, 80(5), e105-e106.
4. Popp, A.J. (2000). Neurosurgical workforce: Examining the physician supply controversy. AANS Bull, 9(1), 7-9.
[aans_authors]







