The COVID-19 national emergency declared in the United States on March 13, 2020, dramatically changed the role of telemedicine in clinical care, since shelter-in-place orders were issued throughout the country. As neurosurgical providers interact with patients in the operating room, intensive care unit, emergency department and outpatient clinics each day, they place themselves as well as their patients at an increased risk of exposure. There was thus a widespread need for further implementation of telemedicine to reduce viral exposure. This manuscript shares the experience and lessons learned at a large tertiary care academic neurosurgery department required to maximally increase telemedicine use as a response to the COVID-19 pandemic.
Methods
A retrospective analysis of patients who received care through the Thomas Jefferson University and Jefferson Hospital for Neuroscience Department of Neurosurgery between Feb. 1 and April 18, 2020, was performed. Patients treated the previous year between March 3 and April 20, 2019, were included as contemporary control. A total of 10,746 patients met the inclusion criteria; the breakdown is displayed in Figure 1. These patients received care by 17 attending faculty (six tumor, five vascular, four spine and two functional attendings) and four nurse practitioners. The COVID-19 national emergency was declared in the United States on March 13, which is used as the reference point in this study. Analysis was carried out using unpaired t-test, Chi-square, Mann-Whitney U test and Fisher’s exact tests. P-values of less than or equal to 0.05 were considered statistically significant. Statistical analysis was carried out with IBM SPSS (Version 24.0. Armonk, NY: IBM Corp.).
Telemedicine Environment
We used the Teladoc Health (Teladoc Health, Purchase, Harrison, NY) and the VidyoConnect (Vidyo Health, Rochelle Park, NJ) telemedicine platforms, integrated to the EPIC electronic health records (EHR) (Epic Systems Corporation, Verona, WI). The telemedicine set-up consisted of one device to remotely access the hospital Internet in order to use the Epic EHR and the telemedicine software and a second device to video conference with nursing staff. The nursing staff was also able to join the physician-patient encounter when necessary or videoconference with the patient independently before or after the physician. This set-up allowed for a 360-degree communication between the neurosurgical team and the patient. Imaging was reviewed with patients using the share-screen functionality of the video-conferencing telemedicine software. When technical issues were encountered, other HIPAA-compliant applications outside of the institution’s bandwidth were used to carry out the telemedicine visit. Additionally, starting telemedicine visits earlier in the day (i.e. 5:30-6 am) helped avoid the network congestion noted later in the day.
Results
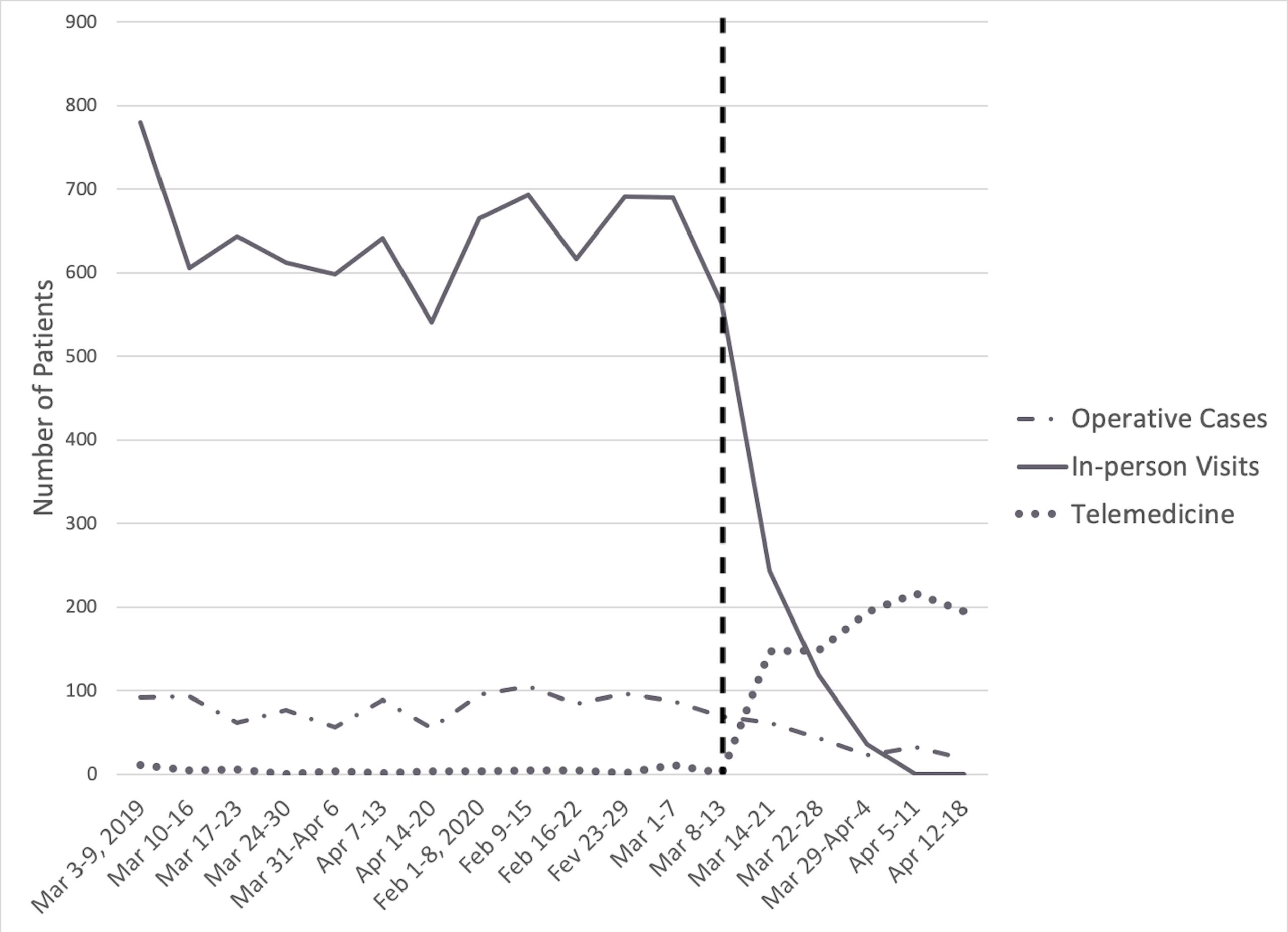
A total of 10,746 patients were included in this study: 1,247 (11.6%) patients underwent surgery, 8,742 (81.4%) were seen in clinic via an in-person meeting and 757 (7.1%) had a telemedicine appointment. The number of patients who had surgery, an in-person clinic appointment or a telemedicine visit during this study period are displayed in Figure 2.
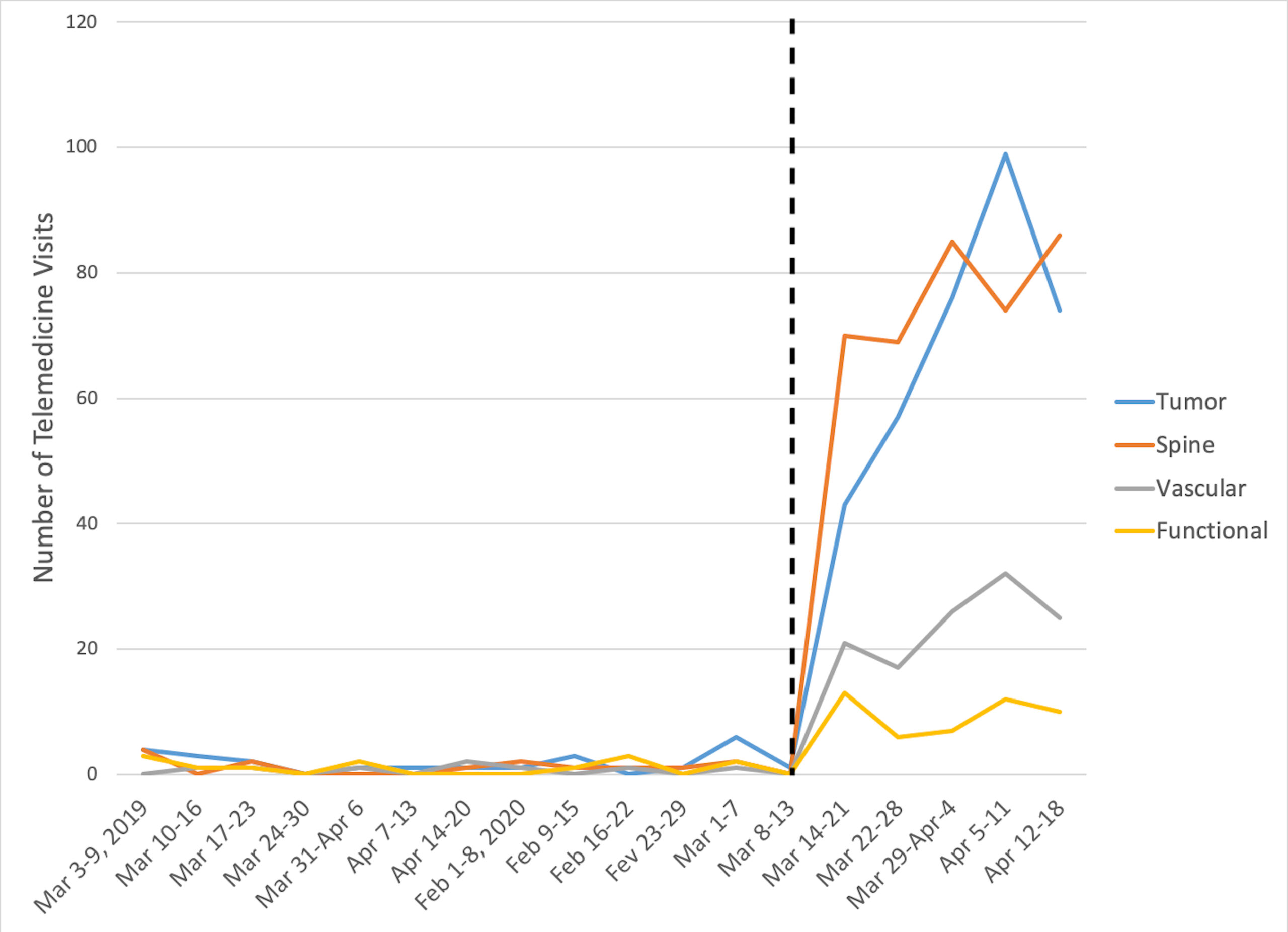
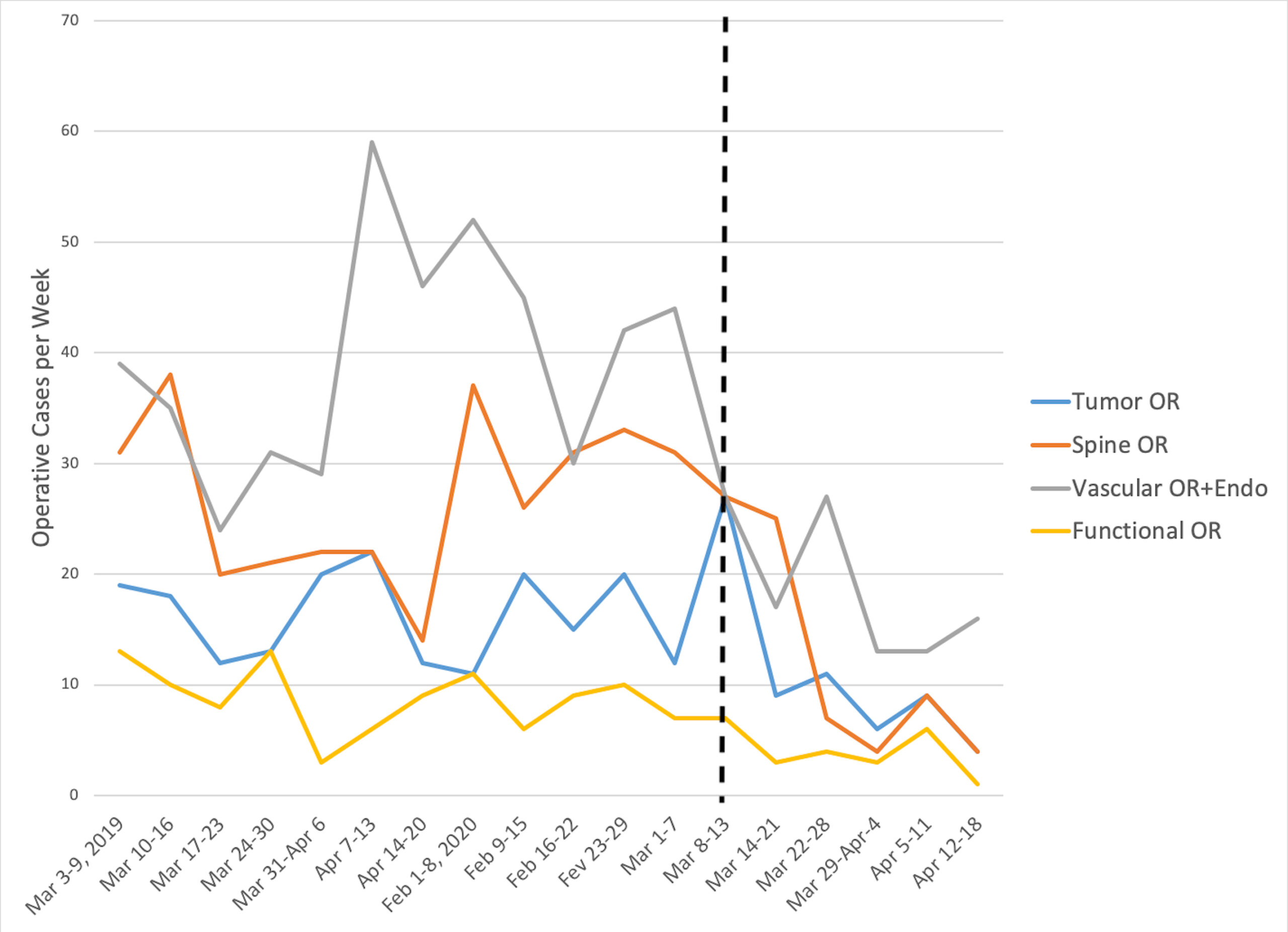
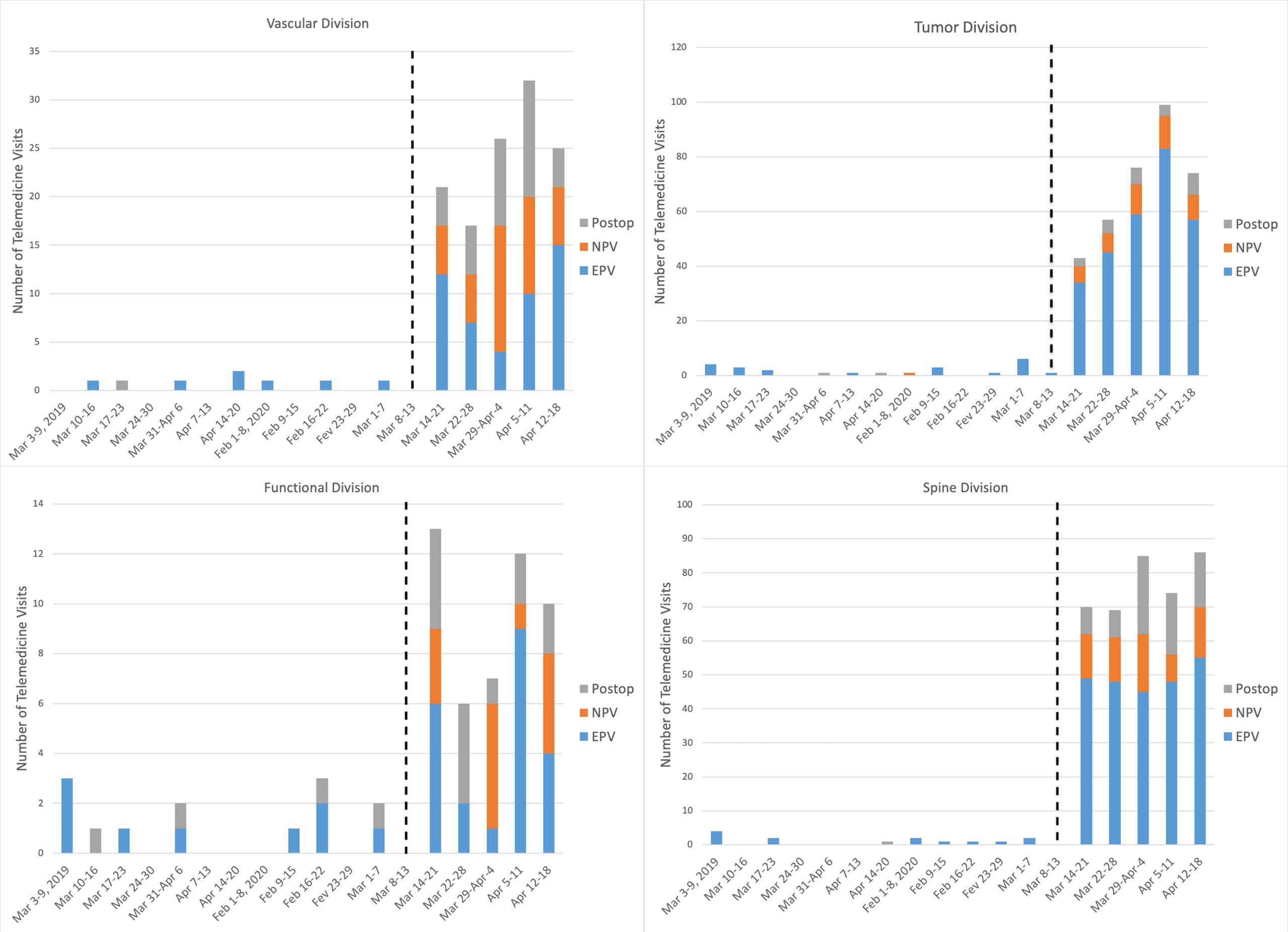
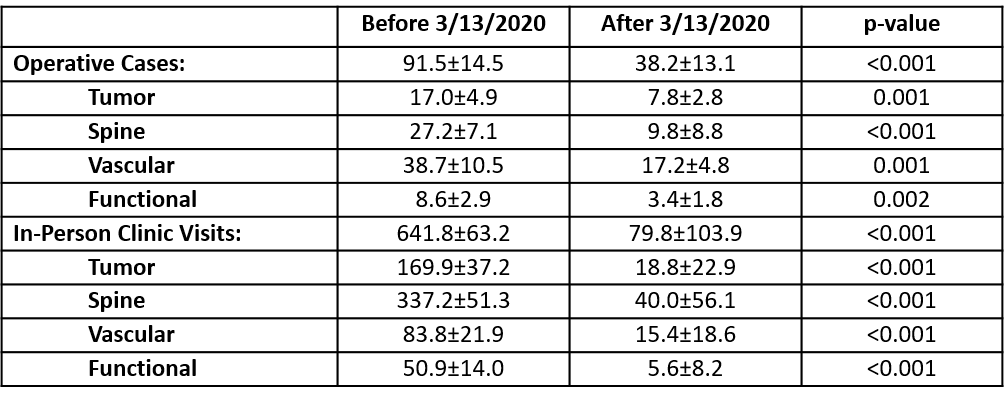
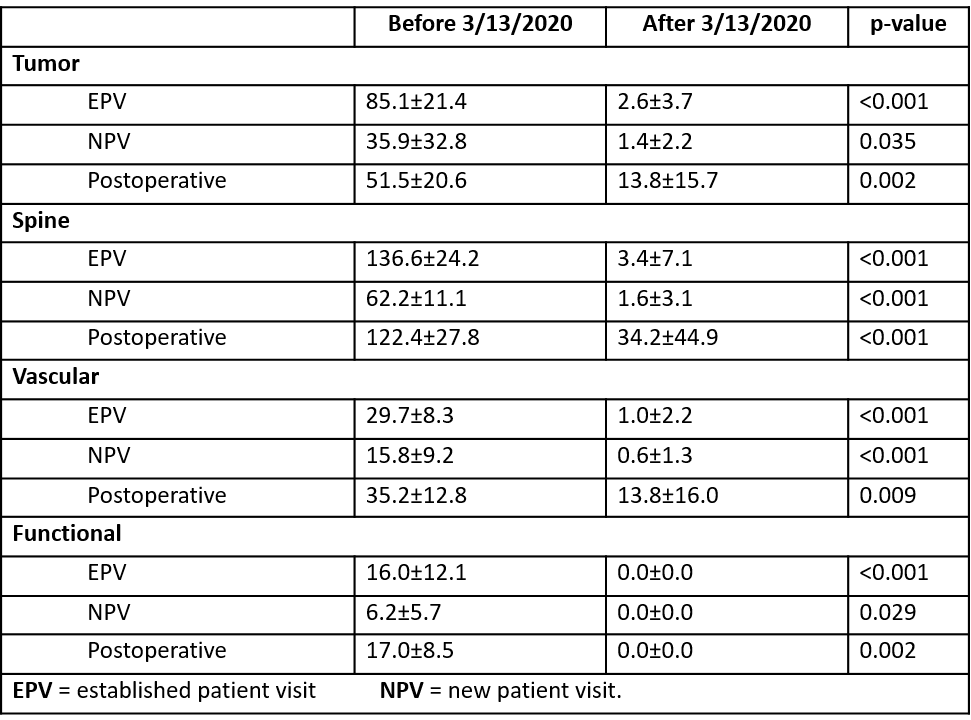
The number of in-person clinic visits per week decreased dramatically from 641.8±63.2 to 79.8±103.9 (p<0.001) (Table 1/Figure 2). The breakdown of visits by division is displayed in Table 2/Figure 3. During the same study period, the number of telemedicine visits per week increased from 4.5±0.9 prior to March 13, 2020, to 180.4±13.9 after March 13 (p<0.001). A statistically significant increase in the number of telemedicine visits was seen in all four divisions, while a statistically significant decrease was noted in the number of operative cases per week in all four divisions (Figure 4). There were no new patient visits performed via telemedicine prior to the shelter-in-place measures, but the number rose significantly across all four divisions to an average of 8.2±2.1 per week after March 13. The proportion of patients who underwent a new patient, established or postoperative follow-up visit in each of the divisions is displayed in Figure 5.
Discussion
The COVID-19 pandemic has tremendously impacted all clinical specialties over the span of a few months. Despite any prior barriers with telemedicine use, our findings demonstrate widespread adoption of this technology through the four divisions.
The rapid expansion of a telemedicine practice is not an easy feat; success is contingent on a strong telemedicine infrastructure. Issues with bandwidth and Internet connection speed were encountered at first as the use of telemedicine was rapidly increased across the enterprise.10 It is very important to estimate the number of new telemedicine users and encounters to sufficiently expand the bandwidth to support the increased use of the platform. We also found that telemedicine not only allowed our staff to provide seamless care to the established and post-operative patients, but also to address new patients who may otherwise avoid seeking care for their health problems in fear of contracting COVID-19. This was feasible due to the 1135 Waiver implemented on March 6, 2020, expanding the coverage of telehealth services by Medicare. Telehealth visits are covered even outside of designated rural areas and they are reimbursed similarly to the equivalent in-person visits for the duration of the COVID-19 national emergency.
The pandemic also highlighted several limitations. While there are a number of companies in this space, there is a lack of telemedicine technology that captures the nuances of the neurological examinations. This has created a tremendous opportunity for the application of artificial intelligence to telemedicine in order to improve our diagnostic and follow-up capabilities. The reimbursement models will also need to be updated in order to incentivize the efficient application of this technology, including new-patient visits.5,8
Not only can telemedicine improve clinic efficiency and patient satisfaction, it can also optimize the surgeon’s schedule. Surgeons can spread out their telemedicine visits throughout the week, including early morning and evening. This strategy could allow the surgeon to expand the number of operative days or free up additional time for academic pursuits. Telemedicine is not likely to diminish the quality of physician-patient encounters, but instead may enhance the relationship by making health care delivery more efficient and convenient. The COVID-19 pandemic forced the widespread adoption of telemedicine. This experience taught us many lessons that we need to learn from to optimize the use of telemedicine in neurosurgery.
Figures
Tables
References
[expand title=”View All”]
1. Chalouhi N, Dressler JA, Kunkel ESI, Dalyai R, Jabbour P, Gonzalez LF, et al: Intravenous tissue plasminogen activator administration in community hospitals facilitated by telestroke service. Neurosurgery 73:662–667, 2013
2. Chhabra HS, Sharma S, Verma S: Smartphone app in self-management of chronic low back pain: a randomized controlled trial. Eur spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 27:2862–2874, 2018
3. Cottrell MA, O’Leary SP, Swete-Kelly P, Elwell B, Hess S, Litchfield M-A, et al: Agreement between telehealth and in-person assessment of patients with chronic musculoskeletal conditions presenting to an advanced-practice physiotherapy screening clinic. Musculoskelet Sci Pract 38:99–105, 2018
4. Goz V, Spiker WR, Brodke D: Mobile messaging and smartphone apps for patient communication and engagement in spine surgery. Ann Transl Med 7:S163, 2019
5. Grossman SN, Han SC, Balcer LJ, Kurzweil A, Weinberg H, Galetta SL, et al: Rapid implementation of virtual neurology in response to the COVID-19 pandemic. Neurology:2020
6. Mouchtouris N, Al Saiegh F, Fitchett E, Andrews CE, Lang MJ, Ghosh R, et al: Revascularization and functional outcomes after mechanical thrombectomy: an update to key metrics. J Neurosurg:1–6, 2019 Available: https://www.ncbi.nlm.nih.gov/pubmed/31518981. Accessed 4 April 2020
7. Neufeld JD, Doarn CR: Telemedicine Spending by Medicare: A Snapshot from 2012. Telemed J E Health 21:686–693, 2015
8. Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M: Evaluating barriers to adopting telemedicine worldwide: A systematic review. J Telemed Telecare 24:4–12, 2018
9. van der Linden SD, Sitskoorn MM, Rutten G-JM, Gehring K: Feasibility of the evidence-based cognitive telerehabilitation program Remind for patients with primary brain tumors. J Neurooncol 137:523–532, 2018
10. Wilcock AD, Rose S, Busch AB, Huskamp HA, Uscher-Pines L, Landon B, et al: Association Between Broadband Internet Availability and Telemedicine Use. JAMA Intern Med:2019
11. Zanaty M, Chalouhi N, Starke RM, Tjoumakaris SI, Gonzalez LF, Deprince M, et al: Epidemiology of a large telestroke cohort in the Delaware valley. Clin Neurol Neurosurg 125:143–147, 2014
[/expand]