Part 1: This is the first article of a two part series describing the authors’ experience working with the NFL’s concussion protocol. Part 2 continues the conversation.
American professional football is the epitome of a contact sport. Inherent in participation is the risk of concussion. Neurosurgery has played a central role in improving the safety of the game and fostering player health for more than 30 years. During that span, it has come into focus that sports concussions are not benign, require proper management and can potentially have long-term consequences. The increased awareness of concussion has caused a shift in behavior, leading to immediate removal followed by active treatment, shortens the length of recovery.1 To improve the diagnosis and management of concussions in its players, the National Football League (NFL) formed its Head, Neck and Spine Committee in 2010, initially co-chaired by neurosurgeons H. Hunt Batjer, MD, FAANS and Richard G. Ellenbogen, MD, FAANS. The committee developed and introduced a set of concussion assessment guidelines in 2013. The “Concussion Protocol” evolved into the current 2019 system of player management. This protocol guides player management both on and off the field by codifying procedures during games and practices, defining the roles of the medical and training staff and setting specific standards for return-to-play. In this article, we describe the NFL Concussion Protocol2 and our experience as neurosurgeons working alongside the head athletic trainer with its implementation and contributions to player health and safety.

The NFL Concussion Protocol
Before each season starts, it is now mandatory that both players and team staff are educated on the importance of recognizing and reporting concussions. All players are also given baseline neurological and neuropsychological examinations. This baseline data includes an extensive concussion history for each player and aids in return-to-play decision making. While teams’ medical and coaching staff still play a primary role in identifying players who may have suffered injury, the Concussion Protocol created several new positions specifically designed to identify and refer players for evaluation. The first is the Unaffiliated Neurotrauma Consultant (UNC). As its name implies, this position is held by a physician impartial and independent from the team. At each NFL game, two UNCs monitor players from the sidelines to aid in identifying those who have potentially suffered a concussion and assist in their evaluation, while a third UNC is in the stadium booth to review video. The second position is the Booth Athletic Trainer-Certified (BATC). These ‘spotters’ are placed in stadium booths with access to multiple views of video and replay during all games to identify potentially concussed players and can call a “medical timeout” that temporarily stops play and removes the player for evaluation. The third additional position is the Independent Neurological Consultant (INC). The INC, also impartial and independent from the team, is utilized during the recovery period from a concussion and must confirm that the player has successfully completed the return-to-play protocol before release to full participation.
Game Day Evaluation
If a player is suspected of having a concussion, it is mandatory that he is removed from the game so the medical team can conduct an evaluation known as the NFL Concussion Assessment. This evaluation is completed by both the team physician and the UNC. The assessment includes:
- Review of “No-Go” criteria, including loss of consciousness, confusion, posturing or amnesia – any of these disallow return to participation until medically cleared
- Inquiry regarding the history of the event
- Review of concussion signs and symptoms
- Maddock’s questions3
- Video review of the injury
- Focused neurological exam
If the player exhibits any of the “No-Go” signs or symptoms, or there is conclusive evidence of a concussion, he is taken to the locker room immediately and cannot return to play or practice until medically cleared. If the evaluation is equivocal, the player is brought to the locker room for the NFL Locker Room Comprehensive Concussion Assessment, which is based on the Standardized Concussion Assessment Tool (SCAT 5).4 The diagnosis of “concussion” or “no concussion” is adjudicated by both the UNC and the team physician. If a concussion is diagnosed, the player is provided an information sheet and instructions for medical personnel contact and follow-up evaluation.
Post-concussion Evaluation
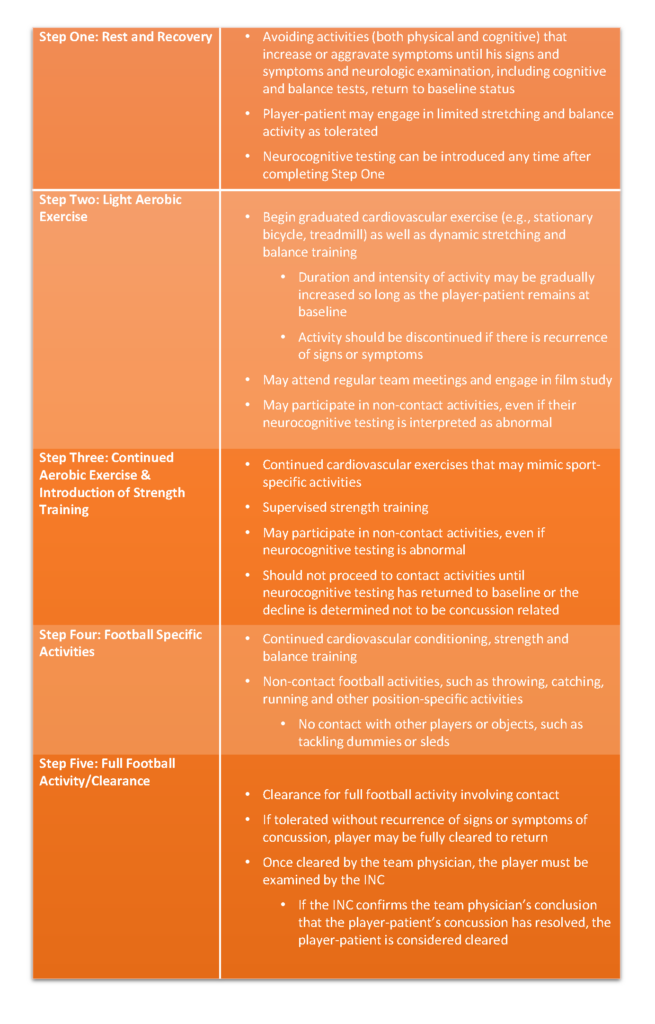
A concussed player-patient is entered into the “Return-To-Participation Protocol,” during which he is monitored at least daily and advances through a stepwise progression of increasing activity (Table 1). Players are disallowed from returning to participation until they have returned to baseline cognitive function and are asymptomatic at rest and during exertion.
Note: Drs. Joseph Maroon, Vincent Miele, and David Okonkwo are members of the Pittsburgh Steelers Football Club Medical Staff; John Norwig is Head Athletic Trainer for the Pittsburgh Steelers Football Club. The views expressed in this article are their own.
Table 1. Return-To-Participation Protocol: Once the player-patient is at baseline level of signs and symptoms and neurological examination, the player may be cleared to proceed to the next step.
Read More in Part 2
References
[expand title=”View All”]
1. Elbin, R. J., Sufrinko, A., Schatz, P., French, J., Henry, L., Burkhart, S., . . . Kontos, A. P. (2016). Removal From Play After Concussion and Recovery Time. Pediatrics, 138(3).
2. (2017, April 05). NFL Head, Neck and Spine Committee’s Concussion Protocol Overview. Retrieved from https://www.playsmartplaysafe.com/newsroom/videos/nfl-head-neck-spine-committees-concussion-protocol-overview/
3. Maddocks, D. L., Dicker, G. D., & Saling, M. M. (1995). The Assessment of Orientation Following Concussion in Athletes. Clinical Journal of Sport Medicine, 5(1), 32-35.
4. Echemendia, R. J., Meeuwisse, W., Mccrory, P., Davis, G. A., Putukian, M., Leddy, J., . . . Herring, S. (2017). The Sport Concussion Assessment Tool 5th Edition (SCAT5). British Journal of Sports Medicine.[/expand]
[aans_authors]